What is Colorectal Cancer?
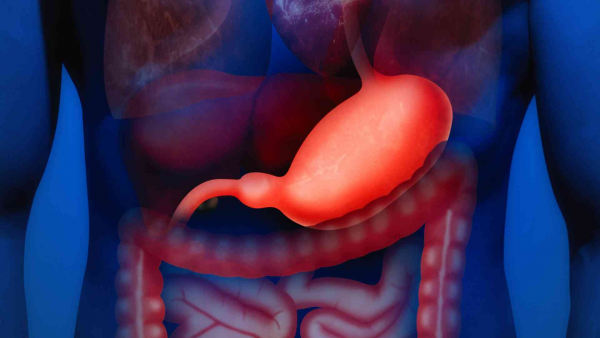
Colorectal cancer, also referred to as "bowel cancer," consists of tumors that develop in the colon (large intestine) or rectum. The colon and rectum (the last 15 centimeters of the large intestine) are essential parts of the digestive system.
Colorectal cancer is the third most common cancer worldwide, with a higher incidence in developed countries.
The impact of diet on colorectal cancer risk is well-established. Factors that increase cancer risk include high consumption of red meat, processed foods, obesity, and low intake of vegetables, fruits, and fish. Chronic constipation and smoking are also known risk factors. Furthermore, a sedentary lifestyle contributes to increased risk.
Both colon and rectal cancer are more common in men. Approximately 61% of cases occur in men and 39% in women. Unfortunately, one-third of patients are diagnosed at a late stage when surgery is no longer feasible.
Colorectal cancer risk increases with age, peaking most commonly in the seventh decade of life. Polyps in the colon increase cancer risk. Individuals previously diagnosed with colon cancer have a higher future risk of developing colon cancer, and women with colon cancer also have an increased risk of developing uterine, ovarian, and breast cancers.
The presence of inflammatory bowel diseases (IBD) also elevates colorectal cancer risk. Both ulcerative colitis and Crohn's disease are associated with increased cancer risk, with ulcerative colitis posing a higher risk. The severity, extent, and duration of these diseases are directly linked to cancer risk. In ulcerative colitis patients, the risk of developing cancer is approximately 3% in the first 10 years, rising to 15% in the following 10 years. The risk is even higher in patients with pancolitis.
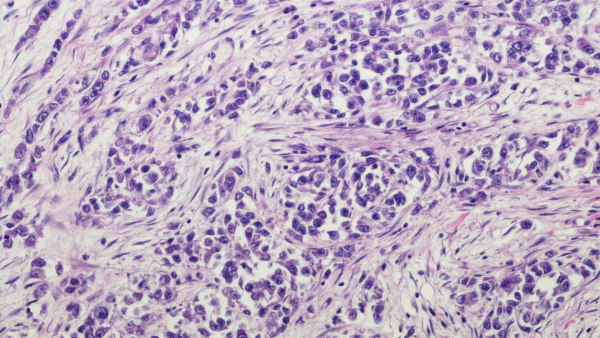
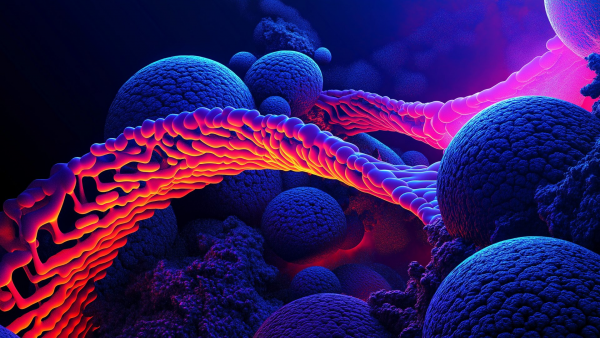
Colorectal cancers develop as a result of abnormal growth and division of cells lining the inner surface of the colon or rectum. These cancers can grow over time and spread to surrounding tissues. Early-stage detection significantly improves treatment success, while late-stage detection worsens prognosis.
Genetic Tests in Colorectal Cancer
Colorectal cancer genetic tests are used to determine an individual's risk of colorectal cancer, understand the genetic causes and prognosis of the disease, identify treatment options, and detect familial cancers to assess the risk in family members. It is recommended that everyone, not only those with a family history of cancer, undergo genetic testing to determine whether they carry a genetic mutation that increases cancer risk.
Colorectal Cancer Genetic Testing Includes:
-
Genetic Counseling: A genetic counselor or specialist evaluates a person's family history and personal risk factors. Detailed family information is collected, including the side of the family with cancer, the number of cases, the age of cancer onset, and types of cancer diagnosed. Information about tests previously conducted on affected family members, their survival status, and the availability of DNA from deceased individuals is also assessed.
Genetic Tests Serve Two Main Purposes:
-
Screening for Hereditary Cancer Predisposition:
This involves screening for genetic changes that may increase cancer risk. The Hereditary Cancer Panel (used in our center) includes approximately 220 genes known to be associated with cancer and 400 candidate genes suspected to be linked to cancer. New cancer genes are added as they are discovered, ensuring that panels remain up to date. Blood samples are collected for this test. The results help individuals better understand their disease risk and make informed decisions regarding early detection and preventive measures. Screening strategies are then planned based on the findings. -
Tumor-Specific Testing for Diagnosis, Treatment, and Prognosis:
Tumor-specific tests can be performed on tissue samples to evaluate colorectal cancer (detailed below) or broader panels can be used.
Tumor Mutation Panel
The Tumor Mutation Panel is a genetic panel test conducted using next-generation sequencing (NGS) technology to assess multiple genetic changes simultaneously. It can be performed on tumor tissue or through a liquid biopsy by analyzing serum obtained from a blood sample. The test evaluates the presence of mutations in numerous genes, as well as microsatellite instability and tumor mutation burden.
These panels provide a comprehensive analysis of the tumor's genetic profile. They help determine the unique characteristics of the tumor, which is essential for identifying personalized treatment options and prognosis. Different centers may offer panels with varying numbers of genes. In our center, we use a panel that includes a broad range of genetic mutations and also evaluates Tumor Mutation Burden (TMB), PDL/PDL1, and Microsatellite Instability. Additionally, polymorphisms associated with the toxic effects and efficacy of classical chemotherapeutic agents are also assessed.
Patients diagnosed with colorectal cancer are strongly encouraged to consult an oncologist and a genetics specialist to evaluate treatment options.
Colorectal Cancer Genetic Screening Tests
-
KRAS (Codons 12, 13, 61, 117, 146) (Next-Generation Sequencing - NGS)
-
NRAS (Codons 12, 13, 61, 117, 146) (Next-Generation Sequencing - NGS)
-
BRAF (V600E) (Next-Generation Sequencing - NGS)
-
MSI (Microsatellite Instability)
-
PIK3CA (Next-Generation Sequencing - NGS) (Exon 9: E542 and E545; Exon 20: H1047)
-
MTOR (for inhibitors)
It is known that KRAS mutations are observed in 35-40% of colorectal cancers, and NRAS mutations in 1-6% of cases. Mutations in codons 12, 13, and 61 are the most frequent. Patients with these mutations are unlikely to benefit from anti-EGFR therapies. Approximately 50% of cases show no mutation and may benefit from anti-EGFR treatment. Comprehensive gene panels may offer access to therapies commonly referred to as "smart drugs".
Family History and Genetic Risk Factors in Colorectal Cancer
Risk factors for colorectal cancer include age, family history, and genetic factors. Therefore, a detailed family pedigree should be obtained, and not only colorectal cancers but all cancers from both the maternal and paternal sides should be considered.
Polyps (Non-Cancerous Tumors in the Intestine)
Polyps are important. Most are benign and harmless, but they result from abnormal cell growth, and some may progress to cancer. A biopsy is used to determine whether a polyp is benign or malignant. If polyps are difficult to access, colonoscopy may be required. A healthy diet, regular exercise, avoiding smoking, and reducing alcohol consumption can help decrease the risk of polyp formation.
Diet's impact on colorectal cancer risk is well-documented. High consumption of red meat and processed foods, obesity, and low intake of vegetables, fruits, and fish increase cancer risk. Chronic constipation, smoking, and a sedentary lifestyle also elevate the risk.
Early Detection of Colorectal Cancer
Early detection is the most important prognostic factor in colorectal cancer. Therefore, regular screening tests are crucial regardless of family history. However, for individuals with symptoms or high risk due to family history, appropriate genetic testing is essential.
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
Chemoprevention is a relatively new concept. In addition to a healthy lifestyle and diet, the use of NSAIDs (aspirin, sulindac, and celecoxib) may prevent disease in high-risk individuals with pre-cancerous lesions and in cancer patients at risk for developing a new malignancy. NSAIDs are an appealing option due to their molecular effects on tumors, their impact on systemic and local inflammatory responses, and their low cost as an adjuvant therapy.
Clinical trial results confirm the effectiveness of NSAIDs in reducing the risk of colorectal adenomas. In the future, a comprehensive anticancer strategy will likely involve more personalized approaches for managing high-risk individuals. However, chemoprevention designed as a long-term, continuous therapy can have adverse clinical effects, and identifying less toxic compounds with well-defined safety profiles is essential.
It is hoped that this new approach will help shift the perception of colorectal cancer from a fatal disease to a manageable chronic condition.
What Are the Symptoms of Colorectal Cancer?
Colorectal cancer symptoms vary depending on the type and stage of the disease. Common symptoms that may occur in the colon or rectum include:
-
Changes in Bowel Habits: Noticeable changes such as prolonged diarrhea or constipation.
-
Bloody Stool: Bright red blood or tar-like stools, often an early sign of colorectal cancer.
-
Abdominal Pain or Bloating: Persistent or frequent discomfort or pain in the abdomen; bloating may accompany this.
-
Unexplained Weight Loss: Loss of weight without any change in activity level.
-
Fatigue and Weakness: Feeling of exhaustion; iron deficiency anemia may also be a sign of colorectal cancer.
-
Nausea and Vomiting: These may also be symptoms of colorectal cancer.
-
Bowel Obstruction: A blockage leading to reduced or absent bowel movements, often due to a tumor.
-
Feeling of Fullness: Sensation of pressure, fullness, or bloating in the intestines.
Remember that these symptoms can also occur in many non-cancerous conditions. Colorectal cancer symptoms can worsen as the disease progresses and spreads. Early detection increases the chance of effective treatment, so individuals with risk factors should have regular health screenings. If symptoms are noticed, it is important to consult a healthcare professional, as early diagnosis and treatment can significantly improve outcomes in colorectal cancer.