Cancer Genetic Tests; can be used to assess a person’s cancer risk, determine its type, and develop a personalized approach for cancer treatment.
With “Cancer Genetic Tests,” it is possible to assess a person’s cancer risk, determine the type of cancer, and develop a personalized approach for treatment.
So what is cancer risk?
What is the incidence of cancer?
Which cancers are most common?
When are we at risk?
When should we worry?
What should we do if we or a family member is diagnosed with cancer?
How much of cancer is genetic?
Which cancers are familial?
What tests should be done in cancer?
Is cancer treatable?
Let’s take a look at these questions that have been on our minds.
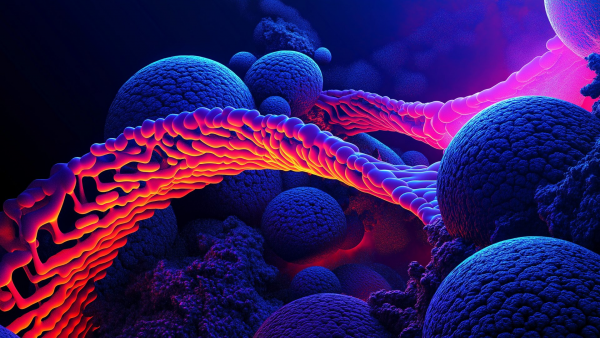
As we complete the first quarter of the 2000s, many concepts about cancer have changed. Cancer is uncontrolled cell proliferation.
It usually starts from a single cell. The incidence of cancer in society is nearly 20%. It can develop spontaneously even without a family history. Thousands of cellular errors occur in our body every day. If these faulty cells are repaired, the problem is solved. If not, the process of controlled cell death (apoptosis) begins to destroy the cell. If apoptosis also fails, the faulty cell starts to proliferate. As it proliferates, this unstable cell undergoes further changes. In fact, the initial error usually does not cause cancer. It is the new changes during cell proliferation that alter the cell’s properties.
It gains characteristics such as increased growth rate, angiogenesis (blood vessel formation), invasion into neighboring tissues, continued division despite contact with neighboring cells, and finally migration to distant organs (metastasis). These new cells have a very different genetic structure compared to the original faulty cell. A process that starts with a single cell spirals out of control. Thousands of genes control this process. Genes responsible for different stages of cell division, apoptosis-related genes, genes regulating interactions between cells, growth and development-related genes, growth-inhibiting genes, gene regulation mechanisms, and immune system-related genes... In short, we are not defenseless. We have a very powerful army protecting us.
Cancer is the second leading cause of death both in our country and worldwide. One in five deaths in our country is due to cancer. Nearly one-third of cancer deaths are directly influenced by our lifestyle, habits, and nutrition. These factors include:
-
Tobacco use
-
Being overweight
-
Low consumption of fruits and vegetables
-
Insufficient physical activity
-
Alcohol consumption
Smoking is responsible for 22% of cancer deaths. Hepatitis and HPV infections are associated with 25% of cancer cases in developing countries. Cancer rates increase with age. In men, the most common cancers are lung, prostate, and colorectal cancers; in women, they are breast, thyroid, and colorectal cancers.
What about genetic factors?
Why doesn't every smoker develop lung cancer? Why do treatment outcomes vary among cancer patients? Can we undergo cancer screening?
First, remember: all cancers are genetic. Uncontrolled cell division means there must be genetic disruption. However, in familial cancers, we inherit a genetic variant related to cancer susceptibility from our parents.
What are cancer genetic tests used for?
Cancer genetic tests can be used to:
-
Assess a person’s cancer risk
-
Determine the type of cancer
-
Develop a personalized treatment approach
-
Provide information on the cancer’s potential treatment response
-
Identify at-risk family members by combining results with family history
As technology advances, we are becoming stronger in early diagnosis, personalized treatment planning, minimizing treatment side effects, and maintaining quality of life during treatment. There are significant differences between our knowledge of genetics 10 years ago and today. One of the major future goals is preventing cancer before it even develops.
Why are these tests important?
We know some people might say:
-
“What will change if I know I will get cancer?”
-
“I will lose morale.”
-
“There’s no solution anyway.”
-
“Knowing will only depress me.”
-
“If you tell me my risk is high, you’ll ruin my life.”
-
“I don't want to know.”
The purpose of this article is to explain why knowing matters.
If a genetic defect associated with cancer is found, does it mean I will definitely get cancer?
Remember, healthy cells only transform into cancerous cells through genetic changes. All cancers involve one or more genetic alterations. However, in about 10–15% of cancers, we inherit a predisposition to cancer via egg or sperm from our parents. These are called hereditary (familial) cancers. Finding a cancer-related variant should not be ignored. Carrying a cancer-related variant does not guarantee cancer development. The risk is determined based on which gene is affected and the type of variant. If you are told, for example, “you have a 50% risk,” this is based on research and clinical data related to that specific gene.
What should someone carrying a variant do?
The information provided by your doctor is crucial. Some gene mutations pose a risk at a young age, while others later in life. Your doctor will collect detailed family history, identify the affected gene, test relatives if necessary, and evaluate the biological mechanisms. Screening strategies, including the method, frequency, and starting age, are then planned accordingly.
Follow-up plans are made for the family based on the results. Some may require early screenings, while others may wait until middle age. Detailed genetic counseling is essential.
We carry two copies of every gene—one from each parent. In familial cancers, a variant is inherited from one parent, and cancer develops if a second mutation occurs in the other gene. This is called the "two-hit hypothesis." Not everyone with a familial variant develops cancer. If the second mutation doesn’t occur or occurs very late, cancer may never develop.
There are genes and variants that particularly concern us because they carry a high risk. Risk levels are explained to individuals after studying population data.
If no cancer-related variant is found, am I still at risk?
If a known familial variant is absent in you, your risk decreases to general population levels. However, sporadic cancers (not familial) still exist. Regular population screenings remain important.
If no family member was available for testing and a familial cancer panel was done but no variant was found, the risk is greatly reduced but not eliminated. Thousands of genes remain unidentified. Therefore, those with multiple family members with cancer, especially those diagnosed before age 50, should still be cautious.
What is NGS (Next Generation Sequencing)?
NGS is a method known as "Next Generation Sequencing." Over the past decade, its success has skyrocketed. It used to be very expensive but has become more affordable. In this method, DNA is extracted, fragmented, libraries are prepared, and sequences are read by machines. Even very low-frequency genetic changes can be detected. This is now the preferred technology for cancer studies.
Can I pass on variants I carry to my child?
Yes, you have a 50% chance of passing genetic mutations to your child. Thanks to current technology, if you carry a cancer-related genetic variant you do not wish to pass on, you can opt for IVF and select embryos that do not carry the mutation.
Today, cancer genetic testing is becoming widely accepted even for those without a family history.
What are cancer genetic tests used for?
Familial cancer screening tests:
Performed with a simple blood draw (in a purple-capped tube), DNA is isolated to search for genetic variants linked to familial cancer, making up 10–15% of all cancers. Early detection through genetic screening can save lives. Results must be interpreted by experienced healthcare professionals.
Cancer tissue testing from a diagnosed tumor:
These tests are used both diagnostically and to guide treatment, by identifying the best therapies and additional options (like immunotherapy or radiotherapy). Tests include:
-
Specific tests for known mutations: (e.g., KRAS in colorectal cancer, ALK in lung cancer)
-
Comprehensive genetic profiling: to detect mutations regardless of tumor type.
Liquid biopsy tests:
When tissue samples are unavailable or new metastases occur, a liquid biopsy from blood can detect tumor DNA fragments. This method is technically demanding and should be done with specialized tubes and minimal delay.
Is there a feature that distinguishes familial from sporadic cancers?
Familial cancers can be suspected when:
-
There is a family history of cancer
-
Cancer occurs at a young age
-
Multiple cancers appear in one individual
-
Multiple tumors occur in the same organ
-
Cancer develops in an unusual gender
-
The cancer has a rare histological type
However, these are not absolute rules.
Should I get genetic testing even if there’s no cancer in my family?
Yes, especially now that broader screening is being recommended. Interpretation of results is as important as testing itself and must be handled by experienced professionals. Genetic counseling is crucial to ensure appropriate follow-up based on test results.
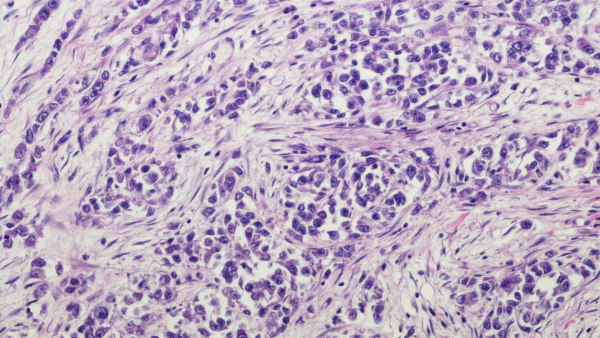
Pathology and Genetics
Pathology and Genetics are inseparable fields when it comes to evaluating tumors. When a tumor is suspected, the tissue is sent to Pathology for histopathological examination. Sometimes, special staining or molecular testing (FISH or molecular methods) is necessary.
Accurate assessment of tumor areas and the percentage of tumor cells is critical for correct interpretation of genetic results. Therefore, close collaboration between pathology and genetics departments is essential.
At Intergen, Pathology and Genetic tests have been performed and evaluated together since 2010.