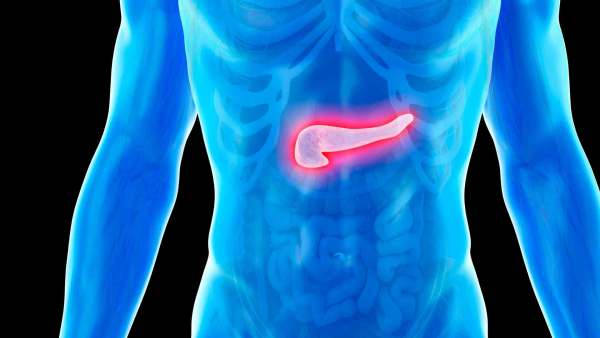
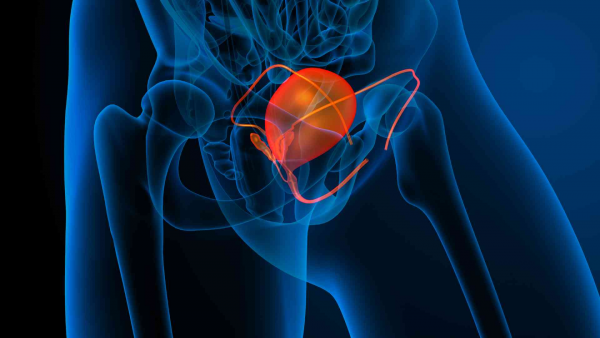
What is Ovarian (Over) Cancer?
Epithelial Ovarian Cancer (epithelial over cancer) is considered the most "hereditary" type of tumor when assessed without selection criteria. In approximately one out of every 4–5 cases, a variant likely to predispose to cancer is found in a gene primarily involved in DNA repair. Advances in DNA sequencing technologies have led to the discovery of additional genes associated with the homologous recombination (HR) pathway, including BRCA1 and BRCA2. Additionally, about 10–15% of epithelial ovarian cancers are known to have a pathogenic variant in the mismatch repair pathway (MMR), which is related to DNA repair. Identifying these variants is crucial in planning chemotherapy regimens and developing targeted therapies.
Variants detected in BRCA and HRR genes are associated with improved progression-free survival when treated with maintenance therapy using poly(ADP-ribose) polymerase (PARP) inhibitors, either as a first-line treatment or in recurrent disease.
Variants in the mismatch repair pathway (MMR) can be detected in the tumor or inherited as a germline variant that predisposes to cancer. Almost half of these cases have been reported to involve variants in the MSH6 gene, as well as in MLH1 and MSH2. When these variants are present, immunotherapies that act on PD-1 receptors affecting the immune system via T cells are used.
Familial Ovarian Cancer:
Approximately 30 out of 100 women with a BRCA1 or BRCA2 gene mutation (higher in BRCA1) are at risk of developing ovarian cancer by age 70.
STK11 gene: Associated with Peutz-Jeghers Syndrome (PJS). Women with PJS have an increased risk of developing a rare type of ovarian cancer known as ovarian sex cord stromal tumors.
Genetic Screening Tests for Ovarian Cancer Risk
These are tests used to assess cancer risk in individuals with a personal or family history of ovarian or related cancers. These tests help understand a person’s cancer risk, determine appropriate preventive strategies, and define screening methods for early diagnosis. They also include pharmacogenetic testing to guide drug selection and dosage decisions. The main test used:
Familial cancer screening tests
Familial (Hereditary) cancer screening panel (Clinicians may use different panels. About 220 genes are known to be associated with cancer, and around 400 are considered “candidate” cancer genes. As new cancer genes are discovered, panels are updated accordingly.)
Genetic Tests in Ovarian Cancer
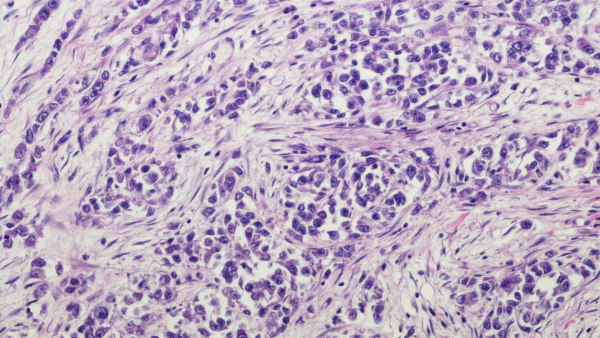
These tests identify specific genetic alterations in a patient’s tumor cells to better understand treatment options and prognosis. The most common genetic tests for ovarian cancer include:
-
BRCA1-2 (Whole Gene Sequencing) (Next Generation Sequencing-NGS) (PARP Inhibitor Sensitivity) (From tissue or blood)
-
HRR genes and HRD scoring studies
-
MSI (Microsatellite Instability): A crucial parameter for immunotherapy eligibility. Routinely screened in ovarian cancer.
-
PD-L1 Immunohistochemistry Test: The presence or absence of PD-L1 protein can guide immunotherapy decisions and help assess the likelihood of response.
-
MMR protein immunohistochemistry staining
-
Tumor mutation panel: A genetic panel test done via NGS (Next Generation Sequencing) that simultaneously tests for various genetic alterations. It can be performed on cancer tissue or via liquid biopsy using serum from a blood sample. This test detects mutations in multiple genes, calculates microsatellite instability and tumor mutation burden (TMB). These panels allow for a detailed genetic profile of the tumor. They help determine the unique characteristics of a patient’s tumor, aiding in the selection of “personalized treatment” options and prognosis. Test content varies between centers. Our center uses a comprehensive panel that includes broad gene screening, tumor mutation burden, PD-L1/PD-1 analysis, and microsatellite instability evaluation. This panel also assesses polymorphisms related to the toxic effects and effectiveness of classical chemotherapeutic agents. Patients diagnosed with ovarian cancer are advised to consult an oncologist and genetic specialist to evaluate treatment options.
RNA Fusion (Gene Fusion) Panel:
This method, known as “RNA seq,” involves extracting RNA from cancer tissue and visualizing all RNAs via NGS to detect fusions and some losses or gains. It plays a crucial role in determining drugs and prognostic markers for selected patients.
Early Diagnosis of Ovarian Cancer
Early detection and treatment significantly increase the success of ovarian cancer treatment, as with all cancers. Since symptoms may appear late, screenings are essential. Therefore, individuals with risk factors should regularly undergo health checkups and seek advice from knowledgeable healthcare professionals.