What Is Bladder Cancer?
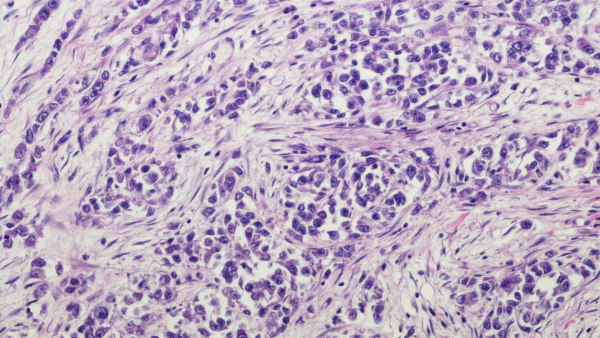
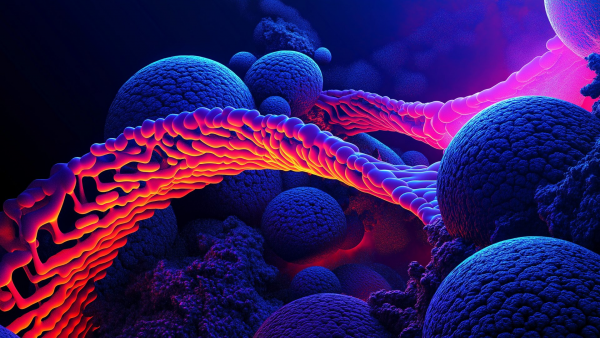
Bladder cancer is a type of tumor that develops in the inner lining of the urinary bladder, the organ responsible for storing urine filtered by the kidneys before it is expelled from the body. It typically arises from the urothelial (transitional epithelial) cells of the bladder lining.
The development of bladder cancer is primarily associated with mutations that activate oncogenes or inactivate tumor suppressor genes. Although men are more likely to develop bladder cancer, women are often diagnosed at more advanced stages and tend to have a poorer prognosis.
Bladder cancer is typically classified into:
-
Non-muscle-invasive bladder cancer (NMIBC)
-
Muscle-invasive bladder cancer (MIBC)
-
Metastatic bladder cancer
As the disease progresses, urothelial cells may transition from non-invasive to invasive forms. Each stage of disease progression involves additional molecular variants and epigenetic abnormalities, which are known to play a significant role.
What Is Genetic Testing for Bladder Cancer?
While environmental exposures such as smoking, occupational exposure to chemicals, and prior chemotherapy/radiation are key contributors to bladder cancer, genetic predisposition and associations with hereditary syndromes like Neurofibromatosis type 2 (NF2) are also known.
Genetic testing can:
-
Identify hereditary cancer syndromes
-
Evaluate cancer risk in individuals
-
Detect specific mutations linked to bladder cancer
These tests are especially considered in cases with family history of cancer or clinical suspicion of a genetic predisposition.
Hereditary Cancer Screening Panels
Hereditary cancer panels commonly include:
-
~220 genes known to be associated with cancer
-
~400 candidate genes under investigation
Panels are updated regularly as new genes are discovered.
Next-Generation Sequencing (NGS) studies have expanded our understanding of somatic mutations involved in bladder cancer. Genetic changes have been observed in:
-
FGFRs,
-
ErbB family,
-
PI3K/Akt/mTOR,
-
Ras-MAPK pathways,
as well as genes involved in chromatin remodeling, cell cycle control, and DNA damage repair.
Of particular note are activating mutations and fusions in FGFR2 and FGFR3, which are targets for precision therapies—making genetic testing from tumor tissue crucial for treatment planning.
Genetic Tests Used in Bladder Cancer
For Urothelial / Bladder Cancer:
-
KRAS (codons 12, 13, 61, 117, 146) (NGS)
-
NRAS (codons 12, 13, 61, 117, 146) (NGS)
-
HRAS (NGS)
-
BRAF (V600E) (NGS)
-
FGFR3 (sequencing – key for FGFR-targeted therapy)
-
PIK3CA (Exon 9: E542 & E545; Exon 20: H1047) – relevant for mTOR inhibitors (NGS)
-
TP53 deletion (FISH)
-
HER2 amplification (FISH)
-
RNA-seq analysis: Used to detect gene fusions (especially in FGFR genes), expression changes, and copy number alterations
Who Should Consider Bladder Cancer Genetic Testing?
Genetic or molecular testing may be appropriate for individuals who have:
-
Symptoms suggestive of bladder cancer
-
A history of smoking or exposure to carcinogenic chemicals
-
Previous pelvic radiation or chemotherapy
-
A family history of cancer
These individuals may benefit from early screening or advanced diagnostics guided by genetic risk assessments.
Symptoms of Bladder Cancer
Symptoms may vary and are sometimes absent in early stages. Common signs include:
-
Hematuria (blood in urine): The most frequent symptom, presenting as pink, red, or cola-colored urine
-
Pain or burning during urination
-
Increased frequency of urination
-
Interrupted urine stream or difficulty emptying the bladder
-
Lower abdominal or pelvic pain
These symptoms are not always cancer-specific and can be linked to other conditions. However, prompt medical evaluation is critical. Early diagnosis significantly improves treatment success. Individuals with symptoms or risk factors should consult a healthcare provider and undergo further investigation if necessary.