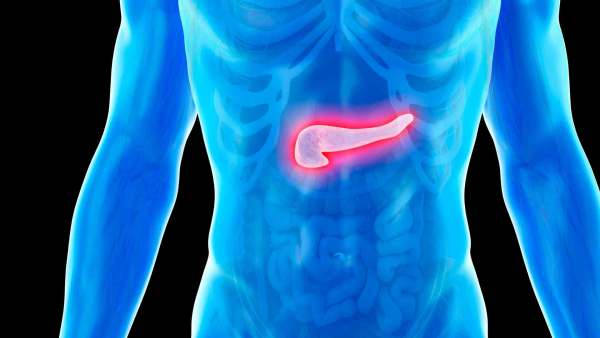
What is Uterine (Endometrial) Cancer?
Uterine cancer (Endometrial cancer) is a type of tumor that originates from the endometrium, the layer of cells lining the inside of the uterus. Endometrial cancer is sometimes referred to as uterine cancer. Other types of cancers can also arise in the uterus, such as uterine sarcomas, which develop from tissues other than the endometrium, but these are much rarer than endometrial cancer. This text discusses both types collectively.
Women who receive estrogen-only hormone replacement therapy after menopause, women treated with tamoxifen for breast cancer, and those who have received pelvic radiation therapy for other reasons (which can lead to cancer 5-25 years post-treatment) are at increased risk of developing uterine cancer. Other risk factors include early menarche (early onset of menstruation), polycystic ovary syndrome (PCOS), obesity, type 2 diabetes, and a personal or family history of breast or ovarian cancer.
Approximately 5% of uterine (endometrial) cancers are considered familial. Mutations in genes responsible for cell growth and DNA repair are associated with uterine cancer. Individuals with a family history of uterine cancer or Lynch syndrome (Hereditary Nonpolyposis Colorectal Cancer - HNPCC) are candidates for genetic testing.
Additionally, women with BRCA and PTEN mutations have an increased risk of developing endometrial cancer. The PTEN gene is associated with Cowden syndrome. Women with Cowden syndrome have an estimated 20-30% lifetime risk of developing endometrial cancer. HRR gene mutations have also been observed in uterine cancers.
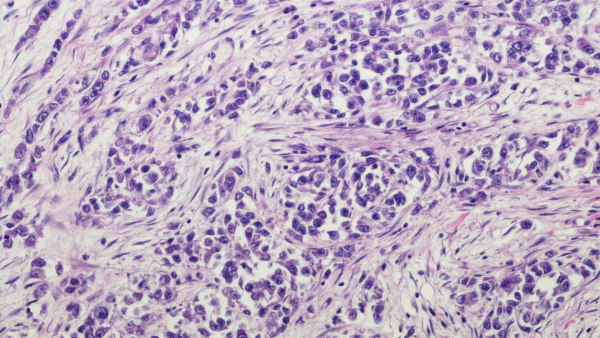
The presence of pathogenic variants in the Mismatch Repair (MMR) pathway, which is involved in DNA repair, is considered an indicator of poor prognosis. MMR mutations are found in approximately 30% of endometrial cancers. These variants also lead to microsatellite instability (MSI). In patients with MMR deficiency, endometrial carcinomas are mostly sporadic, often due to MLH1 promoter hypermethylation or less frequently due to epigenetic silencing of other MMR genes such as MSH2, MSH6, or PMS2. Approximately 3% of patients have an inherited mutation in one or more MMR genes (Lynch syndrome). Screening for Lynch syndrome and identifying patients who may respond to immunotherapy involves assessing MMR deficiency using MMR protein immunohistochemistry (IHC) staining and/or microsatellite instability (MSI) testing.
Lynch Syndrome and Its Relationship with Uterine Cancer
Lynch syndrome is most commonly caused by a pathogenic variant in the MLH1 or MLH2 genes. Variants in MLH5, MSH6, PMS1, PMS2, and TGBR2 have also been linked to Lynch syndrome. These genes regulate cell growth and are involved in DNA damage repair. They are associated with hereditary nonpolyposis colorectal cancer and also increase the risk of developing endometrial cancer. It is known that approximately half of women with Lynch syndrome will develop uterine cancer. Therefore, it is recommended that women with Lynch syndrome begin screening for uterine cancer in their 30s, alongside colorectal cancer screening.
Genetic Screening Tests for Uterine Cancer Risk
These tests are used to assess cancer risk in individuals with a personal or family history of uterine or related cancers, such as ovarian cancer. They help individuals understand their cancer risk, take preventive measures, and establish early detection strategies. Additionally, testing for genes related to drug metabolism helps determine the appropriate medications and dosages for treatment. The following tests are used:
-
Familial Cancer Screening Panel: This hereditary cancer screening panel includes approximately 220 genes known to be associated with cancer and about 400 “candidate” genes suspected of having a cancer association. Clinicians may use different panels. New cancer genes are added as they are identified, and panels are regularly updated.
Genetic Tests in Uterine Cancer
-
BRCA1-2 (Full Gene Sequencing) (Next-Generation Sequencing - NGS) (PARP Inhibitor Sensitivity) (Tissue and Blood-Based): Variants detected in these genes allow for maintenance therapy with poly(ADP-ribose) polymerase (PARP) inhibitors, which improve progression-free survival in both first-line and recurrent disease settings.
-
MSI (Microsatellite Instability): An important parameter for determining eligibility for immunotherapy.
-
Lynch Syndrome Genes (Mismatch Repair - MMR Pathway) (Next-Generation Sequencing - NGS): Identifying variants in these genes is essential for chemotherapy regimen planning and the development of targeted therapies.
-
HRR Genes and HRD Scoring Studies: Variants detected in these genes allow for maintenance therapy with PARP inhibitors, improving progression-free survival in both first-line and recurrent disease settings.
-
PD-L1 Immunohistochemistry Test: The presence or absence of PD-L1 protein can predict the likelihood of response to immunotherapy.
-
Mismatch Repair (MMR) Protein Immunohistochemistry Staining
-
Tumor Mutation Panel: Genetic panel tests performed using NGS (Next-Generation Sequencing) that analyze multiple genetic alterations simultaneously. Tumor mutation panels can be performed on cancer tissue or on serum obtained via liquid biopsy from a patient’s blood. These tests assess mutations across numerous genes, microsatellite instability, and tumor mutation burden. They provide a comprehensive analysis of the tumor’s genetic profile. Such tests help identify the unique characteristics of the tumor, enabling the selection of personalized treatment options and prognosis determination. Different centers offer panels with varying gene coverage. The panel used in our center includes broad gene screening, tumor mutation burden (TMB), PDL/PDL1, and microsatellite instability. It also evaluates polymorphisms related to potential toxicities and drug efficacy of classical chemotherapeutic agents. Patients diagnosed with uterine cancer are advised to consult an oncologist and genetic specialist to evaluate treatment options.
-
RNA Fusion (Gene Fusion) Panel: A method that extracts RNA from cancer tissue and uses NGS to analyze all RNA sequences. It identifies fusions and some losses and gains. "RNA seq" plays a critical role in identifying drugs that can be used for certain selected patients and determining prognostic markers.
Early Detection of Uterine Cancer
Endometrial cancer often presents with symptoms in its early stages. One of the most common symptoms is irregular bleeding. As with all cancers, early diagnosis and treatment significantly improve treatment outcomes for uterine cancer. Therefore, individuals with risk factors should have regular health check-ups and seek counseling from healthcare professionals who are knowledgeable in this field.