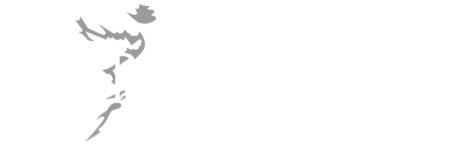
What is Pancreatic Cancer?
Pancreatic cancer is a type of cancer that develops as a result of abnormal growth and proliferation of cells in the pancreas. The pancreas is an organ located between the stomach and small intestine, responsible for producing important substances such as digestive enzymes and insulin. Treatment options typically include surgical intervention, chemotherapy, and radiotherapy.
Symptoms of Pancreatic Cancer
Pancreatic cancer usually does not cause symptoms in its early stages and is often diagnosed at more advanced stages. The symptoms can resemble those of other health issues. However, as the cancer progresses, some common symptoms may include:
-
Abdominal Pain: Pancreatic cancer can often cause pain in the abdominal area, which may also be felt in the back.
-
Weight Loss and Loss of Appetite: Advanced pancreatic cancer can lead to a loss of appetite and significant weight loss.
-
Jaundice (Yellowing of the Skin and Eyes): A pancreatic tumor may block the bile ducts, causing jaundice, which results in yellowing of the skin and eyes.
-
Light-Colored Stools: Blockage of bile flow can cause changes in stool color, making it pale or clay-colored.
-
Dark-Colored Urine: Blockage of bile flow can also cause the urine to appear darker.
-
Nausea and Vomiting: May cause digestive issues such as nausea and vomiting.
-
Blood Sugar Metabolism Problems: Tumors affecting insulin production in the pancreas may cause fluctuations in blood sugar levels and problems with sugar metabolism.
-
Digestive Issues: Can affect the digestive system and cause bowel problems.
These symptoms usually appear in the advanced stages of pancreatic cancer, and because the disease is often not detected in its early stages, it is important to consult a healthcare professional as soon as these symptoms are noticed. Diagnosis typically involves imaging tests, biopsy, and blood tests.
What is Pancreatic Cancer Genetic Testing?
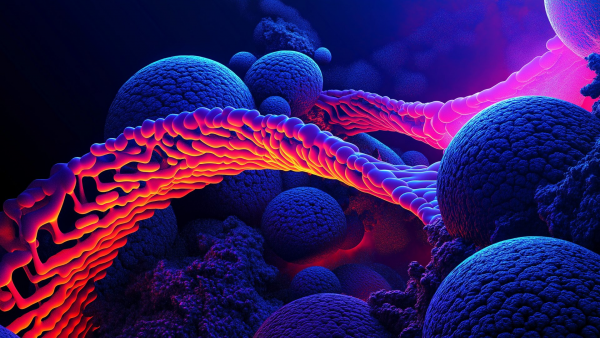
Pancreatic cancer genetic testing is a type of genetic test that examines specific changes in an individual's genetic material (DNA). This test is performed to understand the genetic components of pancreatic cancer and to determine an individual's susceptibility to the disease.
-
Identification of Genetic Changes: Pancreatic cancer genetic testing identifies mutations or changes in specific genes in an individual’s genetic material. These changes can influence a person’s risk of developing cancer.
-
Risk Assessment: The test is also used to evaluate a person’s risk of developing cancer. Genetic testing can be particularly important for individuals with a family history of cancer, as it helps determine genetic predisposition.
-
Hereditary Cancer Screening Panel: Our center’s panel includes approximately 220 genes known to be associated with cancer and around 400 “candidate” genes that are suspected of having a link to cancer. New cancer-related genes are added to the panel as they are discovered, and the panels are kept up to date.
-
Genetic Counseling: Test results can often be complex. Therefore, it is important to receive genetic counseling both before and after pancreatic cancer genetic testing. Genetic counselors help individuals understand their test results and guide them on how to manage this information.
-
Treatment Approaches: Pancreatic cancer genetic testing can also help determine medical treatment approaches. Certain genetic changes may respond better to specific treatments or may make a person eligible for clinical trials.
-
Family Planning: Genetic test results can also provide information about the cancer risk of other family members, which can be important for future family health planning.
Genetic testing is usually recommended and performed by a healthcare professional. However, it is important to remember that genetic testing is not suitable for everyone and should be considered based on individual and family medical history.
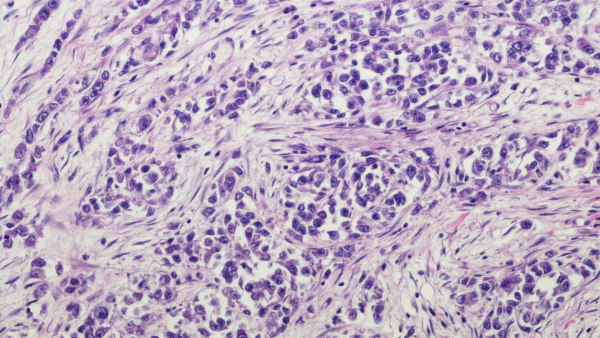
What Genetic Screening Tests Are Used for Pancreatic Cancer?
For Cholangiocarcinoma / Pancreatic Carcinoma:
-
KRAS (codons 12, 13, 61, 117, 146) (Next-Generation Sequencing - NGS)
-
P53 (TP53) (Sequencing Analysis)
-
CDKN2A (Sequencing Analysis)
-
BRCA1-2 (Full Gene Sequencing) (Next-Generation Sequencing - NGS) (PARP Inhibitor Sensitivity) (Tissue-Based)
-
MSI (Microsatellite Instability)
-
PD-L1 Immunohistochemistry Test: The presence or absence of the PD-L1 protein can be a predictor for immunotherapy treatments. This test helps assess the likelihood of response to immunotherapy.
-
Mismatch Repair Pathway - MMR Protein Immunohistochemistry Staining
-
Tumor Mutation Panel: Genetic panel tests performed using the NGS (Next-Generation Sequencing) method, which simultaneously analyzes multiple genetic changes. Tumor mutation panels can be performed on cancer tissue or serum obtained from a patient’s blood via liquid biopsy. These tests examine mutations across numerous genes, calculate microsatellite instability, and assess tumor mutation burden. They provide a more detailed analysis of the tumor’s genetic profile. These tests help identify the unique characteristics of the tumor, determine “personalized treatment” options, and inform prognosis. Different centers may offer tests with varying gene coverage. The panel used in our center includes broad gene screening, tumor mutation burden (TMB), PDL/PDL1, and microsatellite instability. Additionally, the panel assesses polymorphisms related to potential toxic effects and drug efficacy of classical chemotherapeutic agents. It is recommended that patients diagnosed with ovarian cancer consult with an oncologist and genetic specialist to evaluate treatment options.
-
RNA Fusion (Gene Fusion) Panel: This method involves extracting RNA from cancer tissue and using NGS to examine all RNA sequences. It identifies fusions and some losses or gains and plays a critical role in determining potential therapeutic options and prognostic markers for patients.
Who Should Consider Pancreatic Cancer Genetic Testing?
Pancreatic cancer genetic testing is particularly recommended for individuals with certain risk factors. However, there are no strict rules about who should undergo testing—each case should be evaluated individually.
-
Individuals with a Family History: Especially those with a family history of pancreatic cancer in first-degree relatives (parents, siblings, children) may find genetic testing more meaningful.
-
Individuals with a Personal History of Pancreatic Cancer: People previously diagnosed with pancreatic cancer may consider genetic testing, as the results may influence treatment and follow-up plans.
-
Individuals with Specific Genetic Syndromes: Certain genetic syndromes, such as Peutz-Jeghers syndrome, Lynch syndrome, and BRCA gene mutations, may increase the risk of pancreatic cancer. Individuals with these syndromes should consider genetic testing.
-
Families with Multiple Cancer Cases: Genetic testing may be considered in families where multiple types of cancer are common, as the presence of various cancers may indicate a genetic predisposition.
-
Individuals Diagnosed with Cancer at a Young Age: Those diagnosed with pancreatic cancer at an early age may consider genetic testing, as early-onset cancer suggests a possible genetic factor.
In all cases, the decision for genetic testing should be evaluated by a healthcare professional. Genetic counseling is essential for interpreting test results and managing this information. It is important to remember that genetic testing is a tool for determining cancer risk and is not used as a definitive diagnostic method for pancreatic cancer.
What is Cholangiocarcinoma?
Cholangiocarcinoma is a type of cancer that develops in the bile ducts (cholangiocytes). The bile ducts are structures that produce bile, a fluid that helps digest fats. Cholangiocarcinoma often begins with subtle or no symptoms.