What is Breast Cancer?
Breast cancer is a type of cancer that occurs when breast cells grow uncontrollably. It usually originates in the "milk-producing" cells or the "milk ducts" of the breast tissue. While breast cancer predominantly affects women, it can also, though rarely, occur in men.
Genetic Screening Tests for Hereditary Cancer Risk
These tests are used to assess the risk of cancer in individuals who have a personal or family history of breast cancer. It is known that approximately 10% of breast cancers are familial. When a person is diagnosed with cancer, it is important to evaluate whether the cancer is familial, not only for treatment planning but also for determining if other family members are at risk. This assessment is critical for personalized treatment planning for the patient and for identifying at-risk family members, enabling early detection or prevention of cancer in those individuals. Additionally, pharmacogenomic analysis can guide the selection and dosing of medications based on a person’s genetic profile.
These genetic tests investigate variants (mutations) in various genes that may increase breast cancer risk. Primarily, they analyze variants in the BRCA1 and BRCA2 genes, as well as many other cancer-related genes. The test results indicate whether a person carries any high-risk genetic variants.
However, it is important to note that carrying such variants does not guarantee cancer development, nor does the absence of detected variants ensure immunity. These tests are evaluated using data from thousands of sources. If a variant associated with cancer is detected, it must not be overlooked, and an appropriate screening plan should be established based on the specific variant. Considering that at least 80–85% of cancers are sporadic (non-familial), even individuals with no detected variants can still develop cancer. Environmental factors such as smoking, alcohol consumption, and poor diet may further increase this risk.
Genetic Testing for Hereditary Cancer Predisposition
The genetic screening panel for hereditary (familial) cancer risk includes approximately 220 genes known to be associated with cancer and around 400 "candidate" genes suspected of being linked to cancer. Different panels may be used by clinicians. As new cancer-related genes are discovered, they are added to the panels, which are regularly updated.
Genetic Testing in Breast Cancer
Genetic testing in individuals with breast cancer aims to identify specific variants in the cancer tissue. These tests help define treatment options, predict drug resistance, and understand the prognosis by identifying specific genetic changes in tumor cells.
Genetic Tests Used for Breast Cancer Risk
-
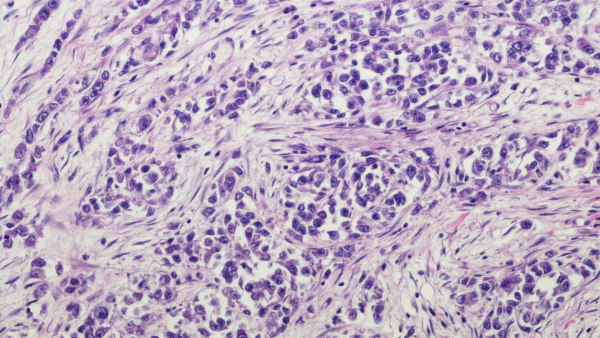
HER2 / Estrogen / Progesterone / Ki67 (Immunohistochemistry Staining)
-
HER2/ErbB2 (FISH)
-
P53 Sequencing (for gain-of-function mutations, to guide radiation dosing)
-
P53 (FISH) (to assess radioresistance)
-
BRCA1-2 (Full Gene Sequencing) (Next-Generation Sequencing - NGS) (PARP Inhibitor Sensitivity) (from tissue and blood)
-
PDL1 Expression Analysis
-
PIK3CA (NGS) (from tissue and blood)
-
HRR Genes and HRD Score Analysis
Genetic Panel Testing:
These are next-generation sequencing (NGS)-based tests that analyze multiple genetic changes simultaneously (tumor mutation panels). They can be performed on tumor tissue or through liquid biopsy from serum obtained from a blood sample. These tests assess mutations across many genes, microsatellite instability, and tumor mutational burden. Panels allow a detailed analysis of the tumor's genetic profile, aiding in identifying the tumor's unique features and informing "personalized treatment" options and prognosis. Different centers offer panels with varying gene counts. Our center’s panel includes comprehensive gene mutation analysis, tumor mutation burden, PDL/PDL1, and microsatellite instability assessment. Additionally, polymorphisms related to the potential toxic effects of standard chemotherapeutic agents and drug efficacy are also analyzed. Patients diagnosed with lung cancer should consult an oncologist and a genetic specialist to discuss treatment options.
RNA Fusion (Gene Fusion) Panel:
This method uses RNA extracted from cancer tissue, analyzed via NGS ("RNA-seq"), to detect fusions and some deletions or duplications. It plays a critical role in identifying potential targeted therapies and prognostic markers for selected patients.
Who Should Undergo Genetic Screening for Breast Cancer Risk?
Breast cancer genetic testing is recommended for individuals with certain risk factors or a family history of breast cancer:
-
Family History: Individuals with a family history of breast cancer may have a genetic predisposition. Testing should be considered for those with first-degree relatives (mother, sister, father, or brother) who have had breast cancer.
-
Carriers of Genetic Mutations: Those known to carry specific mutations such as BRCA1 or BRCA2 should undergo testing, as they have a higher risk of developing breast cancer.
-
Early-Onset Breast Cancer: A personal or family history of breast cancer diagnosed at a young age (e.g., under 40) strongly suggests a hereditary pattern.
-
Other Cancer Types: If there is a history of cancers other than breast cancer—especially ovarian, pancreatic, or other syndromic cancers—genetic testing should be considered to assess hereditary cancer risk (e.g., Li-Fraumeni syndrome).
-
Multiple Cancer Cases: Individuals or families with multiple cancer cases increase the likelihood of genetic testing.
-
Personal History of Breast Cancer: A prior breast cancer diagnosis may indicate a need for testing to evaluate the risk of recurrence.
-
Multifocal Cancer: The presence of multiple tumors in the breast may suggest a hereditary cause.
Additional clinical findings in a patient may also be important. For example, polyps in the gastrointestinal tract, certain thyroid diseases, or benign tumors called hamartomas may indicate a familial cancer syndrome (e.g., Cowden syndrome, Peutz-Jeghers syndrome).
Secondary cancers may develop over time in individuals with hereditary cancer predisposition. Therefore, regular follow-up is essential, particularly for BRCA mutation carriers, where screening for ovarian cancer is critical. (Reports include salivary gland cancer, esophageal cancer, gastric cancer, colon cancer, uterine cancer, thyroid cancer, soft tissue sarcoma, skin melanoma, and acute myeloid leukemia - AML).
Additional risk indicators include ovarian cancer at any age, bilateral breast cancer, multiple breast cancers in the same individual, triple-negative breast cancer (estrogen, progesterone, and HER2 receptor-negative), combined breast/ovarian or pancreatic cancer history in the same family, multiple family members with breast cancer, detected BRCA mutations in family members, and the presence of male breast cancer in the family. In such cases, individuals should be informed about "Hereditary Cancer Screening Tests," and testing should be planned accordingly.
Breast Cancer Genetic Test Results and Their Interpretation
The results of breast cancer genetic tests, whether screening or diagnostic, are highly significant for both the patient and their family. They impact diagnostic interpretation, identification of at-risk family members, and treatment planning for the patient. Results must be evaluated by experienced healthcare professionals, and detailed genetic counseling must be provided. While many cancer-related genes have been identified through next-generation sequencing studies, historically, the BRCA genes were the primary focus when considering breast cancer genetics.
The Importance of BRCA Genes
Approximately 10% of breast cancers are familial. BRCA genes are important in both sporadic and familial cancers. They are involved in DNA repair, and everyone has two copies—one from each parent. A pathogenic variant in one copy confers a predisposition to cancer.
Key Points for Individuals with Positive BRCA Test Results
-
Individuals carrying a BRCA variant have a 50% chance of passing it on to their children.
-
Testing for familial predisposition can be performed using a blood sample. For sporadic cases, testing can be done on tumor tissue or cell-free DNA obtained from a special blood collection tube (liquid biopsy).
-
Approximately 50% of women with BRCA mutations develop cancer by age 70. (The risk is 59–87% for BRCA1 mutation carriers and 33–80% for BRCA2 mutation carriers).
-
The risk of developing cancer is higher in families with a history of breast cancer, and the risk of a second cancer is also increased for those with a BRCA mutation.
-
Men with a BRCA1 mutation have an increased risk of prostate cancer, while those with a BRCA2 mutation have an increased risk of breast cancer. Male relatives should also be screened.
-
In BRCA mutation families, breast cancer tends to occur at younger ages (≤50 years) and shows a more aggressive clinical course.
-
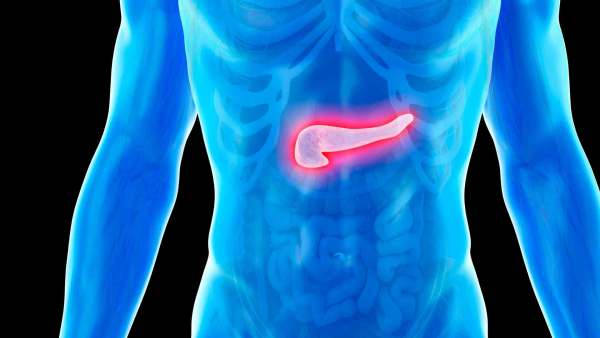
Both male and female BRCA1/2 mutation carriers, although at lower risk, are also at an increased risk for pancreatic cancer and should be monitored.
-
Specific BRCA variants have been associated with certain blood disorders, such as Fanconi anemia, particularly in children inheriting a pathogenic variant from both parents. Counseling should include information about this risk.
Benefits of Genetic Testing
-
Identifying Genetic Susceptibility: Genetic tests can detect specific mutations or changes that may increase an individual’s risk of breast cancer. Particularly important mutations, such as those in the BRCA1 and BRCA2 genes, should be interpreted by experienced physicians, and detailed genetic counseling should be provided.
-
Personalized Medical Advice: Test results guide personalized medical recommendations. Depending on the gene and the variant’s effect, appropriate screening programs and protocols are established. For instance, if a mutation is detected in a DNA repair gene, it should be considered when planning radiotherapy and during screening.
-
Early Diagnosis and Monitoring: Genetic test results enhance individual awareness and encourage proactive health management. Regular screenings can lead to early detection, which is life-saving.
-
Personalized Treatment Options: Genetic test results play a critical role in tailoring treatment strategies for patients diagnosed with breast cancer. Treatment choices, including hormone receptor or targeted therapies, are often guided by genetic profiles. These tests are essential and among the first performed after a cancer diagnosis. They are highly valuable. For hormone receptor-negative patients, advanced testing becomes even more crucial.
-
Continued Scientific Advances: As the understanding of these diseases grows, so does the development of genetic and immunological advancements for both diagnostic and therapeutic purposes. Staying up-to-date is essential, as any new discovery that can impact even one person’s life is invaluable.