What is Papillary Thyroid Cancer (Thyroid Carcinoma)?
Papillary thyroid cancer is the most common type of thyroid cancer, accounting for approximately 80% of all thyroid cancers. The thyroid gland is an important organ located in the neck, responsible for producing hormones such as thyroxine (T4) and triiodothyronine (T3) that regulate metabolism. Papillary thyroid cancer originates from the cells of this gland. Approximately 3-4% of non-medullary thyroid cancers are familial. It is more common in women and typically occurs at younger ages in women compared to men.
This type of cancer usually grows slowly and has a better prognosis than other types of thyroid cancer.
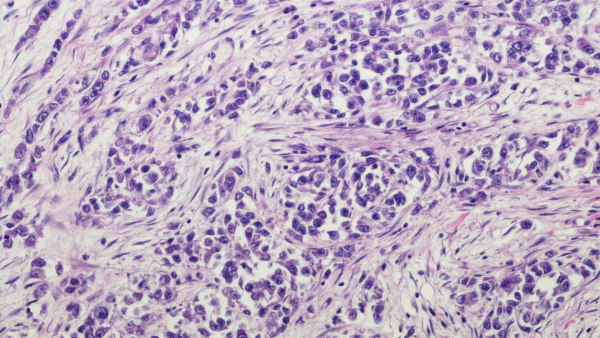
Characteristics of Papillary Thyroid Cancer
Key features of this type of cancer include:
-
Stem Cell Origin: Papillary thyroid cancer originates from the stem cells of the thyroid gland. These cells are essential for the production of thyroid hormones.
-
Well-Defined Nodules: It typically presents as well-defined nodules (small lumps) within or around the thyroid gland.
-
Slow Growth: This cancer type generally grows slowly and rarely spreads to nearby lymph nodes or other organs.
-
Radiation Exposure: The risk of developing papillary thyroid cancer is higher in individuals exposed to high doses of radiation to the head and neck, especially during childhood.
Genetic Tests in Papillary Thyroid Cancer and Risk Assessment
Genetic testing is a medical test performed to assess a person’s risk of papillary thyroid cancer or to identify genetic factors that may predispose them to the disease. Papillary thyroid cancer originates from the cells of the thyroid gland and is the most common type of thyroid cancer.
-
Detection of Genetic Mutations: This test aims to identify specific genetic mutations associated with papillary thyroid cancer. Mutations in genes such as BRAF, RET/PTC, and RAS have been linked to papillary thyroid cancer.
-
Risk Assessment: Genetic testing is important for determining whether there is an association with certain rare genetic syndromes. A portion of familial cases may be part of specific syndromes. For example:
-
FAP (Familial Adenomatous Polyposis Coli), associated with colon cancer.
-
Cowden Syndrome (Multiple Hamartoma Syndrome), related to the PTEN gene, which can involve benign tumors affecting the breast, thyroid, and uterus.
-
Carney Complex Type 1, associated with the PRKAR1A gene, where benign tumors, hormonal issues, and increased risk for papillary and follicular thyroid cancer may occur.
-
Gardner Syndrome, Werner Syndrome, and DICER1 Syndrome can also be associated with non-medullary thyroid cancers.
-
Additionally, there are families with multiple affected individuals where no known syndromes are identified—these families may carry unidentified cancer susceptibility genes. Research has also indicated potential associations with genes on chromosome 1 and chromosome 19 in familial non-medullary thyroid cancers.
-
For these reasons, it is recommended that individuals diagnosed with papillary thyroid cancer be carefully evaluated for signs of these associated conditions, and genetic testing should be planned if necessary.
-
Treatment Planning: Genetic test results can influence treatment decisions. In some cases, more aggressive treatment or the use of specific drugs may be required.
-
Family Counseling: Genetic testing results can also help assess the cancer risk for family members. Those with a family history of similar cancers may consider genetic testing for themselves.
Genetic Screening Tests Used for Papillary Thyroid Cancer
These tests are performed on tumor tissue to investigate somatic changes that develop within the cancer.
-
KRAS (codons 12, 13, 61, 117, 146) (Next-Generation Sequencing - NGS)
-
NRAS (codons 12, 13, 61, 117, 146) (Next-Generation Sequencing - NGS)
-
HRAS (Next-Generation Sequencing - NGS)
-
BRAF (V600E) (Next-Generation Sequencing - NGS)
-
RET Rearrangements (FISH - Breakapart)
Symptoms of Papillary Thyroid Cancer
Symptoms of papillary thyroid cancer are usually related to the growth of the thyroid gland in the neck or the presence of a thyroid nodule. However, these symptoms can also be caused by other thyroid conditions or benign (non-cancerous) nodules.
-
Neck Lump: A swelling or lump in the neck, especially in the thyroid area. This lump is typically painless.
-
Thyroid Nodule: Papillary thyroid cancer often presents as one or more nodules (small lumps) in or around the thyroid gland.
-
Throat Discomfort: A feeling of discomfort in the throat, which may be due to a thyroid nodule or cancer in the neck area.
-
Difficulty Swallowing: An enlarged thyroid gland or nodule may cause difficulty swallowing.
-
Voice Changes: Cancer can affect the vocal cords, leading to changes in voice quality.
-
Growth of a Nodule: The enlargement or more prominent appearance of an existing thyroid nodule.
-
Neck Pain or Tenderness: While usually painless, some patients may experience mild pain or tenderness in the neck area.
-
Swollen Lymph Nodes: In some cases, cancer may spread to lymph nodes in the neck, causing them to become enlarged.
Papillary thyroid cancer typically grows slowly, and symptoms in the early stages may be mild. Therefore, individuals who notice any changes in the thyroid gland or any suspicious symptoms in the neck area should consult a healthcare professional.